Venous Insufficiency

What is Venous insufficiency?
Venous insufficiency is a type of venous disease that occurs when the veins in your legs become damaged. This makes it more difficult for blood to flow through them, causing it to pool in your legs. When this disease occurs over a long period of time, it is known as chronic venous insufficiency (CVI). Over 25 million Americans have varicose veins, which may be an early sign of venous insufficiency. Of those affected, nearly 2.5 million have gone on to develop CVI.
If left untreated, CVI can cause other chronic health problems, including skin problems and open sores (ulcers). While it is not life-threatening, CVI can be a painful and debilitating condition. Understanding what the signs of CVI are can help you get the treatment you need from a vascular specialist.
How Do Veins Work?
In order to understand how venous insufficiency develops, it is important to first learn about the three main types of veins in our bodies — deep veins, superficial veins, and perforating veins.
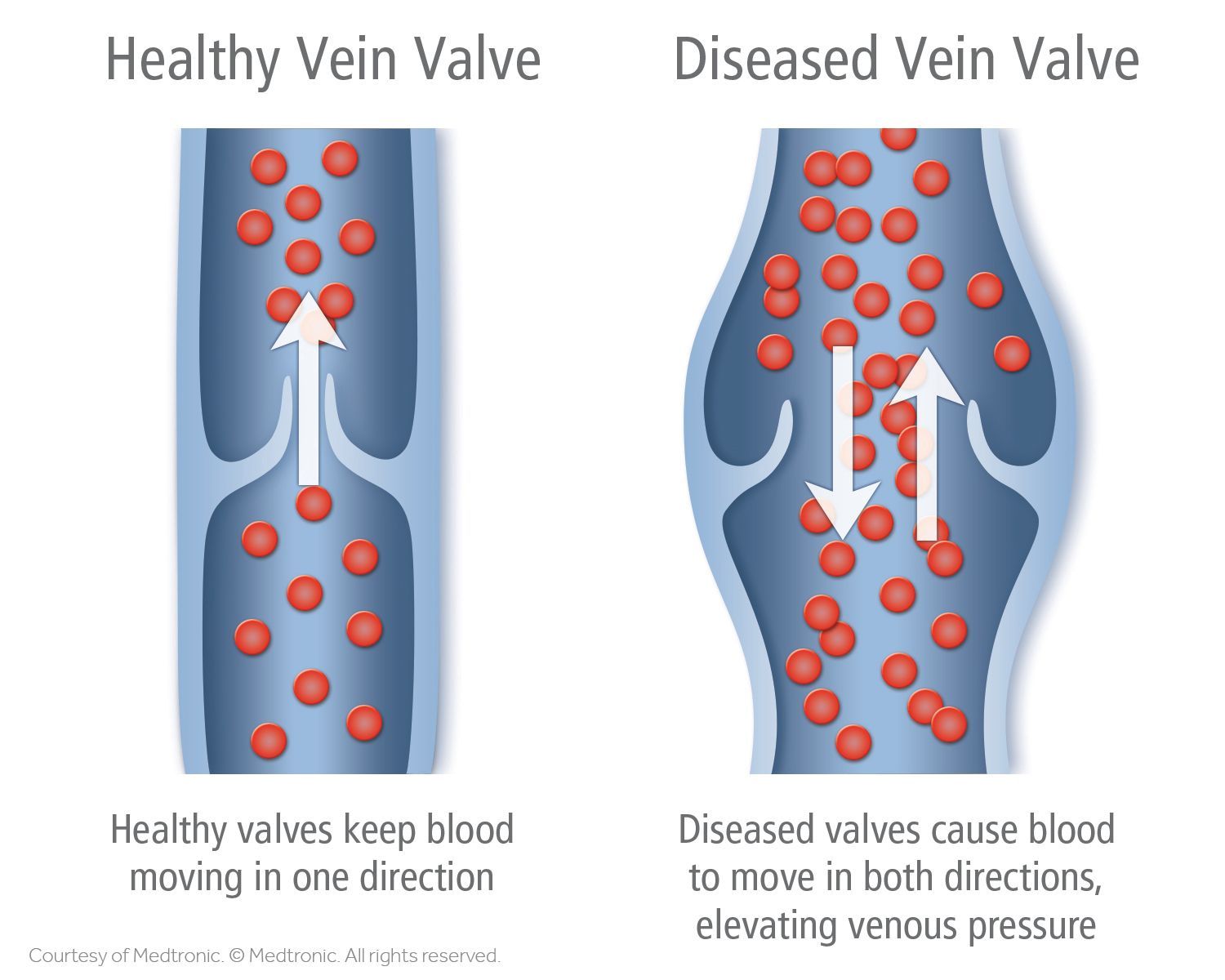
Deep veins are the largest in your body and are found inside your muscles. These veins have specialized valves in them that allow blood to flow only one way through your body. This ensures it moves in the right direction to reach your heart.
Superficial veins are smaller than deep veins and are found closer to the skin’s surface. They also have valves that help ensure blood moves from your tissues back to your heart and lungs. These veins are responsible for carrying blood from tissues near the skin back into your deep veins from the perforating veins. Unlike deep veins, superficial veins are not controlled by muscles, so blood moves more slowly through them.
Perforating veins are the short passageways that connect the superficial veins to deep veins. These veins contain valves that close when your muscles contract to prevent blood from the deep veins from flowing backward into the superficial veins (known as venous reflux).
How Do Leg Veins Work?
Your heart is responsible for pumping the oxygen-rich blood from your lungs out to other parts of your body. So, how are these veins able to carry the oxygen-depleted blood from your muscles and tissues back up to your heart?
Most people do not know that they have a “second heart” that works against gravity to help move blood back up. The muscles in your lower legs act as a powerful pump — every time you take a step, your body weight presses down on the deep veins in your foot. This causes the blood in these veins to travel upward toward your calf. Your calf muscle then squeezes as you lift your heel, which keeps the blood moving upward toward your thighs and your heart.
This “second heart” only works when you’re walking and moving blood from your feet upward. Without the added pressure, blood moves through your feet and legs more slowly — this increases your risk of venous diseases, including CVI.
What Is Venous Insufficiency?
Venous insufficiency is caused by faulty valves in your leg veins that prevent blood from flowing back up to your heart. When these valves are damaged, it causes blood to pool in your feet and legs. This results in increased pressure in your legs, which can lead to uncomfortable symptoms and potential long-term damage.
Doctors and researchers worked together to develop a classification system for CVI. This is known as the Clinical, Etiology, Anatomic, Pathophysiology (CEAP) classification to help doctors diagnose and treat CVI. There are seven stages of venous insufficiency that are based on vein changes and symptoms experienced. These include:
- Stage 0: Achy or tired legs, with no visible symptoms
- Stage 1: Spider veins and other visible blood vessel issues
- Stage 2: Varicose veins that are at least 3 millimeters (mm) wide and can be felt under the skin
- Stage 3: Leg swelling (edema) without any skin changes
- Stage 4: Leg swelling with skin changes, including thickening, and color or texture changes (known as lipodermatosclerosis)
- Stage 5: Previously open sores or ulcers that have healed
- Stage 6: Active ulcers
CVI is diagnosed at stages 3 and above. Varicose veins are not considered CVI, but they are a sign of potential vein issues. If you notice any new varicose veins, let your doctor know or book an appointment with a vein specialist. They can help you address any problem veins before they become worse.
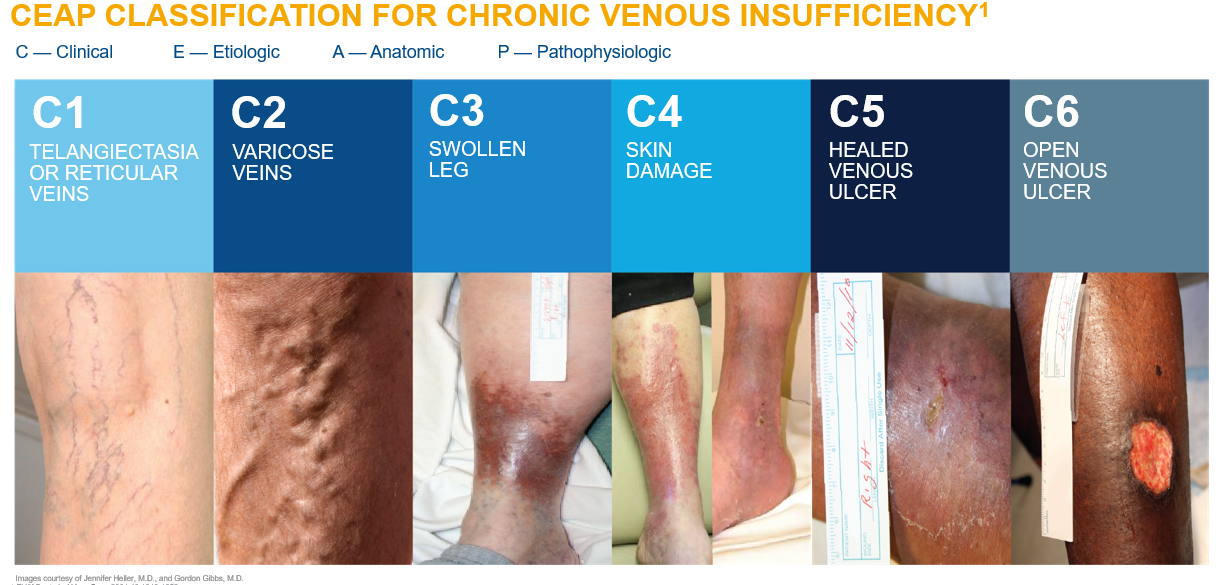
Chronic venous insufficiency (CVI) is a vein disease characterized by swelling, skin damage, and open wounds (ulcers) on the skin. CVI develops slowly over time as a result of faulty valves. The disease is staged using a classification system based on symptoms and vein changes. While spider veins are not considered CVI (which is diagnosed at stage C3), they still may be a sign of potential issues later on.
If you notice any new spider veins, talk to your doctor or book an appointment with a vein specialist. They can help you address any new problem veins before they become worse.
To learn more about venous insufficiency,
read here.
What Causes Venous Insufficiency?
Veins and valves are most often injured from dilation or widening of the vein. Other factors can contribute to an increase in pressure in the legs, further damaging the valves.
The most common cause of this damage is deep vein thrombosis (DVT), or the formation of a blood clot in a deep vein in the body. The blood clot blocks blood flow, causing pressure to build up behind it, which widens the vein. Even if the clot is removed or dissolves, it can create scar tissue that permanently damages the vein. You are at an increased risk of CVI if you have a personal or family history of DVT.
Other causes of CVI include:
- Weight gain or obesity: weight gain from pregnancy or being overweight or obese can put extra pressure on the veins in your legs, damaging the valves
- Sitting or standing for too long: immobility decreases blood flow from the feet and legs toward the heart because the “second heart” is not pumping as much as it should
- Surgery or leg injury: these may block blood flow in a leg vein, causing an increase in pressure; you may also walk less when recovering from surgery or a leg injury, which slows blood flow back to the heart
Women are at an increased risk of developing CVI due to hormone changes. Estrogen and progesterone are known to make collagen fibers relax, which can contribute to blood vessel widening. Studies show that this may increase the risk of blood clots (venous thrombosis), varicose veins, and venous insufficiency, particularly during pregnancy.
Some people are born with vein disorders (known as congenital disorders) that may not be diagnosed until later in life. Others may also have peripheral arterial disease (PAD), which causes narrowing of the leg veins. Most people with PAD have atherosclerosis or the buildup of fatty plaques in their blood vessels that causes blockages. The symptoms of PAD may overlap with those of CVI, and many people have both conditions. Your doctor will talk to you about your treatment options and any extra precautions you need to take when living with both CVI and PAD.
How Do You Know If You Have Venous Insufficiency?
Symptoms of CVI develop over time, and you may notice one or more symptoms before you are diagnosed. These include:
- Varicose veins, or enlarged blue veins close to the skin’s surface
- “Pins and needles,” tingling, or burning sensations in your legs and feet
- Tired or aching legs
- A feeling of heaviness or fullness in your legs
- Leg cramping at night
- Swelling in the ankles and lower legs, typically at the end of the day or if you have been standing for an extended period of time
- Itchy, flaky, dry skin on your feet or legs
- Red or brown skin that has a leathery texture on your feet, ankles, or shins
- Open sores that do not heal over time (known as venous stasis ulcers) that appear around the inner ankle, outer ankle, or shin
How Is Venous Insufficiency Diagnosed?
Venous insufficiency is often diagnosed with a physical exam. Your doctor will look at your feet and legs and ask about any symptoms you are experiencing. They will look for any skin changes, including color changes, swelling, or ulcers. They will also take your medical history — it is important to tell your doctor if you have a family history of venous disorders or DVT in yourself or your family.
Your doctor may also use an ultrasound to look for any damage to your veins. A common technique used is Doppler ultrasound, which measures sound waves bouncing off the red blood cells moving through your veins. This helps your doctor visualize how blood is moving in your body. Specifically, your doctor will likely use duplex ultrasound.
During the procedure, your doctor will spread a gel on your leg and place a wand (transducer) over where they believe there may be a damaged blood vessel. The transducer sends sound waves into your body, which are then recorded and turned into images that your doctor looks at. They may also press down on your leg to see if blood begins pooling or flowing backward. In total, a Doppler ultrasound can take 30 minutes to one hour to complete.
Treatments for Venous Insufficiency
First-line treatments for venous insufficiency focus on compression therapy to help move blood from your feet and legs. Your doctor will also advise you to make lifestyle changes that can help reduce swelling and prevent future complications. Overall, the goal of treatment is to treat pain and swelling, improve your skin health and appearance, and heal any ulcers or wounds you may have.
Compression Therapy
Compression therapy uses specialized compression garments that apply extra pressure to your feet, ankles, and legs. They help prevent blood from pooling in your legs, which treats CVI symptoms. Compression garments are made to apply different amounts of pressure, depending on how severe your CVI case is. Many people wear these garments in the long term to help control their CVI and prevent ulcers and swelling from returning.
Compression Stockings
There are several types of compression garments used to manage CVI. Compression stockings are the most common — these long socks apply the most pressure at the ankle and gradually lessen as they move up the leg. They are made to apply different levels of pressure depending on your needs. Compression stockings are available as knee-high or thigh-high garments. In more severe CVI cases, your doctor will prescribe special stockings that fit your specific measurements. These are commonly used in people with venous ulcers or for those who stand for extended periods of time throughout the day.
Compression Bandages
For those with venous ulcers, doctors typically recommend compression bandages. These are long pieces of elastic wrap that are wrapped around the ankles and legs by a doctor or nurse. To help treat ulcers, you may have a dressing placed under the compression bandages to absorb any fluids and promote healing. Compression bandages must be kept clean and dry, so they are changed once or twice a week.
Intermittent Compression Pumps
If your CVI cannot be properly managed with compression stockings or bandages, your doctor may recommend using intermittent pneumatic compression (IPC) pumps. These pumps mimic the effects of the “second heart” in your legs by squeezing your calves to promote blood flow back up to your heart. IPC pumps are used for several hours throughout the day to help reduce swelling and other CVI symptoms.
Using Compression Therapy
Many people experience discomfort when they first begin compression therapy. This is normal and it should improve as you continue to use stockings, bandages, or IPC pumps to reduce swelling. If you are having a difficult time sticking to treatment, talk to your doctor and they can offer advice or recommend new compression methods. Elevating your feet and legs above your heart while using compression therapy can help reduce extra swelling.
If you also have PAD, be sure to let your doctor know — compression therapy may be more harmful rather than helpful in this case.
Medications
Medications for CVI help treat ulcers, keep skin moisturized, and prevent blood clots associated with the disease. Your doctor may prescribe antibiotics to treat infected ulcers. A daily dose of aspirin can also be used to help ulcers heal faster.
Topical steroid creams or ointments may be applied to the skin or a medicated bandage to treat irritated and inflamed skin (known as stasis dermatitis). Your doctor will recommend using scent-free, gentle moisturizers to treat itchiness. Be sure to avoid heavily scented or anti-itch products, as these can irritate the skin more or even cause an allergic reaction.
If your CVI was caused by DVT or a blood clot, your doctor may have you take an anticoagulant (blood thinner). These medications prevent your blood from clotting by interfering with proteins known as clotting factors. The most commonly prescribed blood thinners are warfarin (Coumadin, Jantoven) and direct oral anticoagulants (DOACs). To learn more about blood thinners for DVT, read here.
Minimally Invasive Treatments
Minimally invasive vein treatments are also used to close off dysfunctional veins, preventing blood from flowing backward and pooling in your legs. A specially trained vein specialist may use sclerotherapy, radiofrequency ablation, or a phlebectomy to treat superficial veins close to your skin. These procedures use local anesthesia and make a small incision near the vein. They are associated with little to no downtime for healing.
Sclerotherapy uses a thin needle to inject a chemical solution into a dysfunctional vein, causing it to collapse in on itself. The vein remains in your leg, but it can no longer carry blood to your deep veins. To learn more about sclerotherapy, read here.
Radiofrequency ablation uses a long, thin tube known as a catheter with a specialized tip on it that creates high-frequency radio waves to heat up a vein. This procedure seals the vein internally so it can no longer carry blood to your deep veins. Nearly all patients see success with this treatment for several years. To learn more about radiofrequency ablation, read here.
A phlebectomy can be used to remove varicose veins near the surface of your skin. Your doctor will create very small incisions to access the dysfunctional vein, then use a hook to remove it. To learn more about phlebectomy, read here.
Surgical Treatments
In CVI cases where medication and minimally invasive treatments do not work, surgery may be used. The goal of vascular surgery is to tie off dysfunctional veins so they can no longer carry blood, or remove them entirely from your body. Depending on the location of the dysfunctional vein and how large it is, your vein specialist may perform ligation and stripping.
This surgical procedure involves making large incisions to access the dysfunctional vein to tie it off (ligation). They can then remove the vein through the incision (stripping). This is an effective treatment for CVI involving large veins in the leg. Stripping and ligation require you to be under general anesthesia and have a longer recovery time than minimally invasive procedures.
Living with Venous Insufficiency
If you are living with CVI, there are steps you can take to prevent it from becoming worse or returning. These lifestyle changes promote better blood flow from your legs back to your heart. They also help prevent the return of uncomfortable symptoms that make recovery difficult.
Health professionals from New York University recommend getting active whenever you can to help your “second heart” pump blood. Just 30 minutes of walking or using a stationary bike several days a week can help improve circulation in your calves and thighs. Stretching your leg muscles can also promote better blood flow.
Exercising or regular movement can also help you maintain a healthy weight. Excess weight puts extra pressure on the veins in your legs, which can weaken them over time. Following a healthy diet that is limited in salt can be beneficial. Diets high in salt cause your body to hold onto water, which raises your blood pressure.
Frequently Asked Questions (FAQ)

DR. AMIT POONIA M.D.
Your New Jersey Vein Specialist
Dr. Poonia is double board-certified in interventional pain management and anesthesiology.
Dr. Poonia’s philosophy is based on teamwork, cooperation, and collaboration among his patients’ treatment teams. He believes that healthcare providers work
best when they work together to accurately diagnose a patient’s problem, find effective treatments, and provide maximum rehabilitation and quality of life improvements.
Dr. Poonia customizes his treatment plans based on each patient’s unique characteristics. He employs the latest minimally-invasive technologies to enhance comfort during treatment and to speed recovery.
References
- Chronic Venous Insufficiency. Cleveland Clinic. July 17, 2022. Accessed January 15, 2023. https://my.clevelandclinic.org/health/diseases/16872-chronic-venous-insufficiency-cvi.
- Doppler Ultrasound. MedlinePlus. December 15, 2020. Accessed January 15, 2023. https://medlineplus.gov/lab-tests/doppler-ultrasound/.
- Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2014;130(4):333-46. doi:10.1161/CIRCULATIONAHA.113.006898
- Khilnani NM, Min RJ. Imaging of venous insufficiency. Semin Intervent Radiol. 2005;22(3):178-184. doi:10.1055/s-2005-921950
- Lifestyle Changes for Chronic Venous Insufficiency. NYU Langone Health. Accessed January 16, 2023. https://nyulangone.org/conditions/chronic-venous-insufficiency/treatments/lifestyle-changes-for-chronic-venous-insufficiency.
- Matic M, Matic A, Djuran V, et al. Frequency of peripheral arterial disease in patients with chronic venous insufficiency. Iran Red Crescent Med J. 2016;18(1):e20781. doi:10.5812/ircmj.20781
- Peripheral Arterial Disease. Centers for Disease Control and Prevention. December 19, 2022. Accessed January 15, 2023. https://www.cdc.gov/heartdisease/PAD.htm.
- Ropacka-Lesiak M, Kasperczak J, Breborowicz GH. [Risk factors for the development of venous insufficiency of the lower limbs during pregnancy–part 1]. Ginekol Pol. 2012;83(12):939-42.
- Scovell S. Patient Education: Lower Extremity Chronic Venous Disease (Beyond the Basics). UpToDate. September 20, 2021. Accessed January 15, 2023. https://www.uptodate.com/contents/lower-extremity-chronic-venous-disease-beyond-the-basics.
- Serra R, Gallelli L, Perri P, et al. Estrogen receptors and chronic venous disease. Eur J Vasc Endovasc Surg. 2016;52(1):114-18. doi:10.1016/j.ejvs.2016.04.020
- Veins. Cleveland Clinic. June 19, 2022. Accessed January 15, 2023. https://my.clevelandclinic.org/health/body/23360-veins.
- Venous Insufficiency. MedlinePlus. May 10, 2022. Accessed January 15, 2023.
https://medlineplus.gov/ency/article/000203.htm.